New Method Could Help Find Potential Treatments for Rare Diseases
January 5, 2019
Finding treatments for rare diseases is difficult: Because they affect such a small number of people, research funding and other resources may be limited. Even if researchers are interested in studying a rare disease, the methods for testing potential drugs may not yet exist. A major focus at NCATS is to identify ways to test compounds and therapies that could apply to a wide range of rare disorders.
Scientists in NCATS’ Assay Development and Screening Technology (ADST) program are collaborating with rare disease organizations to find better ways to test possible drugs for rare diseases. Scientist Mike Iannotti, Ph.D., spent three years as an ADST postdoctoral fellow developing a new way to measure whether a potential drug is effective against the inherited disease alpha-1 antitrypsin (AAT) deficiency. His fellowship was funded by the Alpha-1 Foundation, an organization founded by people with AAT deficiency, a disease that can cause serious lung and liver problems.
The work has not yet led to a new treatment for AAT deficiency, but it should help speed the process of finding treatments for that and many other diseases—both rare and common.
New Tests for Potential Drugs

A robot retrieves compound plates from storage incubators (right) and brings them to a transfer station (foreground) where compounds are transferred to assay plates.
ADST scientists use a technique known as high-throughput screening, in which robots carry out many experiments at in hundreds or even thousands of tiny wells that fit on a plastic plate that is the size of an index card. Scientists refine the tests—called assays—used in high-throughput screening so that they meet specific needs.
However, finding the right assays to use in testing for potential drugs against diseases can be difficult. Scientists often need to test large collections of thousands of compounds to see whether any of them affect a disease.
“For many rare diseases, not only do we not have any drugs that work, we don’t even have any assays that can be used to search for such drugs,” said ADST Director James Inglese, Ph.D., who supervised Iannotti’s work. “Rare diseases sometimes don’t have obvious targets for compounds and drugs compared to many widely studied diseases, such as cancer and cardiovascular disease.”
Many existing assays will not work for rare diseases because of their unique underlying biology. In some cases where rare diseases share a similar biology, scientists can develop new assays specific to several diseases at the same time. Such assays can tell scientists whether a compound or drug has a promising effect on a disease.
A Focus on AAT
Healthy liver cells make the protein AAT and then secrete it into the blood. The protein travels through blood vessels to coat the lungs, protecting healthy tissue from potential attack by immune cells.
In people who have AAT deficiency, the protein does not form properly. Some people get liver disease because the protein builds up and forms toxic clumps inside the liver cells. Others can develop lung disease because they do not have enough AAT to protect their lungs. Patients can receive AAT intravenously, but this only slows the progression of lung disease, and no treatment currently exists for liver disease.
Iannotti’s goal was to develop an assay to test the effects of small molecules as potential drugs on cells that model AAT deficiency. If a small molecule were to change how AAT is released, he would know that it is worth investigating. He needed to be able to measure how much AAT the cells were producing.
Measuring the amount of protein coming from cells is straightforward if researchers test one potential drug at a time; however, NCATS’ high-throughput screening library contains approximately 400,000 small molecules, so Iannotti needed a way to test many of them at once.
He began working with a kind of cell that is relatively easy to grow in the laboratory and can be altered with common genetic engineering tools to mimic a disease. He introduced AAT with a mutation found in many people with AAT deficiency and fused it with a protein that glows. By measuring the glow, he could see how much AAT protein was coming out of the cells.
Measuring Protein with a New Plate
The technique worked, but Iannotti wanted a better way to measure the amount of protein coming from a cell.
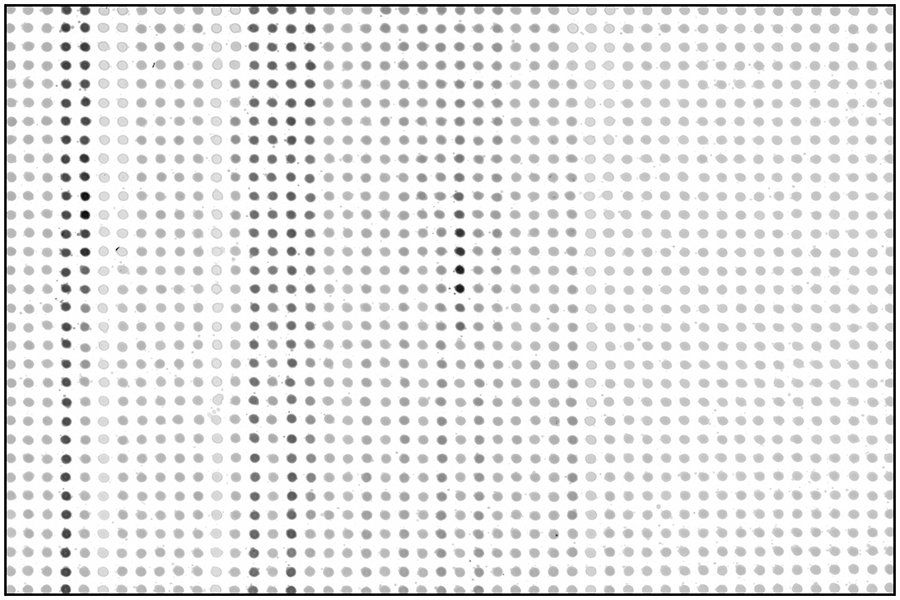
A new NCATS-designed assay plate allows protein samples to be measured through tiny dots of liquid.
“It really bothered me that we couldn’t measure secreted protein in a straightforward, cost-effective way without modifying the cell with a glowing protein,” Iannotti said. “It’s like trying to compare how fast two people can move when one of them is dragging a suitcase.”
To measure the unmodified AAT protein directly in a high-throughput setting, Iannotti realized that he needed an assay plate that could hold a sheet of nitrocellulose, a substance that is part of a common process for detecting individual proteins because proteins stick to it. Once the proteins are on a sheet of nitrocellulose, a researcher can cover it with molecules that bind only to the protein of interest. Those molecules, in turn, can be made to glow.
The idea worked. NCATS’ Automation and Compound Management group stepped in to create a new prototype assay plate that snapped together to hold a nitrocellulose sheet. That allowed Iannotti to measure unmodified protein on the nitrocellulose sheet through 1,536 tiny dots of liquid to determine how much protein was in each dot. He and his colleagues recently described the method in the journal ACS Chemical Biology.
A Method for Many Diseases
The new method that Iannotti developed still has several steps to go before it can lead to a treatment for AAT deficiency. Iannotti still needs to run the tests with cells that are more like the liver cells of people with AAT deficiency. Through the Alpha-1 Foundation, he has access to stem cells developed from patients with AAT deficiency to test potential drugs.
Researchers at NCATS and elsewhere also could use the new method to study many other diseases. “Cells that secrete proteins include everything from insulin-producing cells to cells shedding viruses,” said Inglese. “It would be great to be able to measure that process in a very effective, efficient way.”
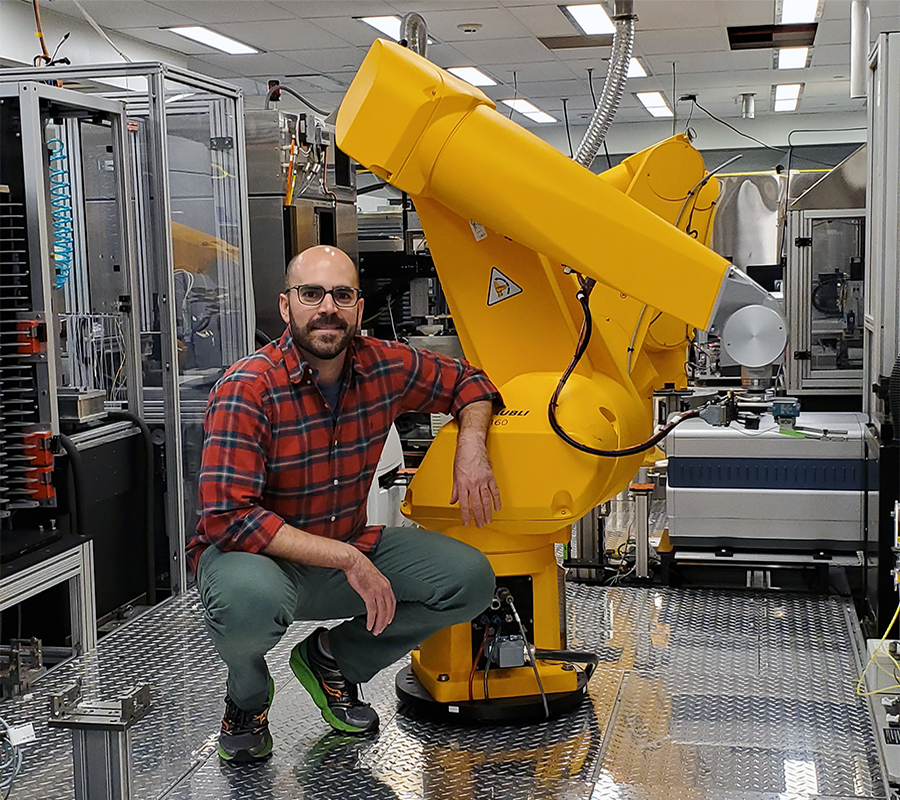
NCATS scientist Mike Iannotti, Ph.D.
A New Research Path
For Iannotti, the Alpha-1 Foundation’s fellowship has opened up new translational research—and career—opportunities. “NCATS has provided me with translational research training in a unique environment, with its resources, expertise, and access to automation and compound screening facilities. It has enabled me to be innovative and design experiments in a different way than was possible as a graduate student,” he said.
Iannotti and the foundation both benefit from the fellowship. “The foundation gets a rare disease champion who focuses on its disease. At the same time, I’ve been able to tackle a real-world problem and accomplish my research goals.”
Working with rare disease patients and families has changed his perspective.
“Sometimes as researchers we’re so focused on our work in the lab, we lose sight of the people with the rare disease we’re studying,” he said. “We started with a blank slate, and we worked together to establish a research path forward to eventually help those with a rare disease.”