CTSA Program-Supported Researchers May Turn Brown Fat into an Ally Against Obesity
March 23, 2021
Researchers funded by NCATS’ Clinical and Translational Science Awards (CTSA) Program have applied translational science approaches to expand the understanding of brown fat in humans as a potential therapeutic target for blunting obesity’s deadly impact on people’s cardiovascular and metabolic health.
The findings appeared in the January issue of the journal Nature Medicine. The study’s lead author, Tobias Becher, M.D., and corresponding author, Paul Cohen, M.D., Ph.D., worked on the study as part of the Laboratory of Molecular Metabolism at The Rockefeller University in New York.
In the human body, white fat stores excess energy, disturbs glucose and lipid metabolism, and fuels obesity. In contrast, brown fat burns energy to generate heat when the body senses cold, and it may play a positive role in the body’s use of glucose. Although everyone begins with brown fat at birth, not everyone maintains it as they grow older. Even among those who keep it, brown fat levels drop with age.
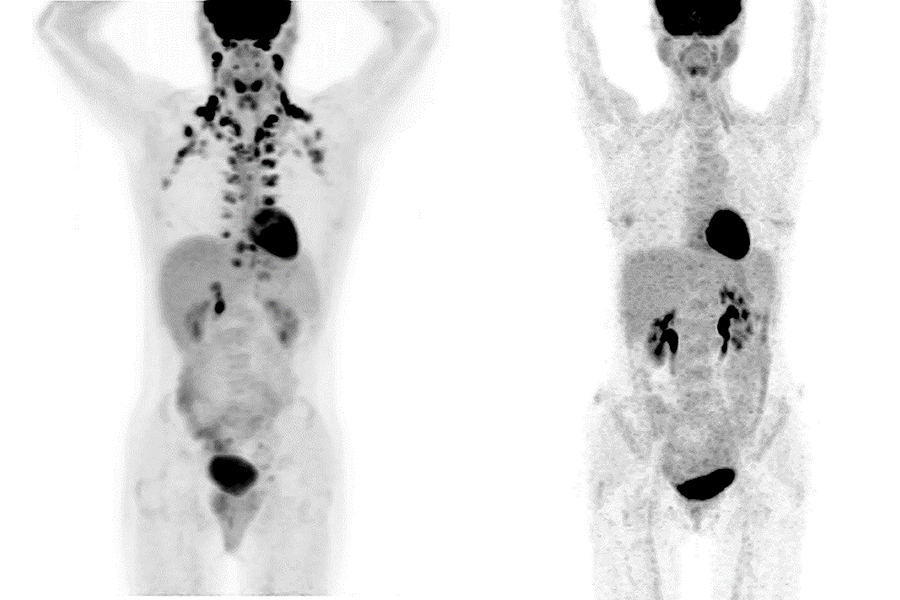
Preliminary research has pointed to the possibility that adults with brown fat may enjoy some cardiovascular and metabolic protection because of it. These findings were based on small studies, and robust assertions about brown fat’s protective possibilities require far more data. The problem is brown fat isn’t easy to measure. Positron emission tomography (PET) scans pick up brown fat’s presence, but relatively few people are ever likely to undergo such an expensive, invasive scan that involves radiation exposure.
PET scans are routinely used in cancer diagnosis and care, so the Rockefeller University scientists reached across medical-specialty boundaries — and literally across a Manhattan street — to collaborate with their colleagues at the Memorial Sloan Kettering (MSK) Cancer Center.
Between June 2009 and March 2018, MSK had collected 134,529 PET–computed tomography (PET/CT) reports from 52,487 patients. MSK also had electronic health records rich with the patients’ medical history, including cardiometabolic information.
Becher and his team electronically searched the scans for the presence or absence of brown fat. The investigators then matched those scans with available clinical data for each patient, including cancer types, use of medications, weight, and the presence of diabetes and cardiovascular conditions.
“The large amount of data that was accessible from MSK and the linkage to the electronic health records gave us a huge database to explore these associations that we had hypothesized at the beginning,” Becher explained.
As a member of the Clinical Scholars master’s degree program at The Rockefeller University, Becher’s translational science training paired his clinical knowledge with team-based tools to make connections that otherwise would have gone unlinked.
“His training allowed Tobias to employ high-level biostatistics and to collaborate with very experienced biostatisticians at the Rockefeller CTSA to analyze the data,” Cohen noted. “Without those kinds of links and collaboration, this research work would never have come together.”
The researchers found that the odds of having cardiovascular and metabolic disorders were lower when patients had brown fat. For example, after accounting for cancer-related factors, MSK patients with brown fat had 56% decreased odds of having type 2 diabetes. They also had 14% lower odds of having high cholesterol and triglycerides, 32% lower odds of coronary artery disease, and 15% lower odds of having high blood pressure. Even after adding obesity to the equation, brown fat’s protective effects still didn’t disappear. Obese patients who had brown fat had lower odds of cardiometabolic conditions than those without brown fat — especially when it came to type 2 diabetes, coronary artery disease and congestive heart failure.
How can medicine manipulate brown fat levels and activity to improve people’s cardiometabolic health? The Rockefeller University translational scientists say the next research steps will have to untangle the effects of environment, genetics and aging.
It’s known that exposure to cold and aerobic exercise activates brown fat. Could drugs moderate brown fat’s activity as well? It’s also known that brown fat levels plummet with age, which may partially explain why people tend to become cold more easily as they get older. New research also could reveal the role genetics plays in determining who keeps brown fat and who loses it over time.
Whatever the next steps, they will employ the same translational science approaches that helped brown fat leap from an energy-burning oddity to a promising therapeutic ally to improve public health.